Picture an ICU where clinicians have instant access to every critical piece of patient information, seamlessly integrated from all medical devices and hospital systems; where the need to manually document clinical information in multiple systems is a rarity. That is not a futuristic vision. Rather, it’s the power of interoperability. And it’s already a reality in many hospitals around the world that have implemented a clinical information system designed for high interoperability.
This article explores the essence of interoperability, its importance for critical care clinicians, and the hurdles in achieving it. It also describes how a clinical information system can meet the challenges and deliver on the promise of high interoperability in critical care and beyond.
What is interoperability in healthcare?
The Healthcare Information and Management Systems Society (HIMSS) defines interoperability as the ability of varied information systems, devices, and applications to access, exchange and integrate data, and to collaboratively use it in a coordinated manner. The goal is to provide timely and seamless portability of information within and across organizations, regions, and countries, so that clinicians have the right information at the right time to make the best possible decisions for patient care.
HIMSS further notes that it is crucial that system architectures, device and application interfaces, and communication standards are designed to allow data to be accessed and shared appropriately and securely across the complete continuum of care. This is known as “full exchange of data”.
Why hospital interoperability is crucial in the ICU and beyond
The seamless data exchange made possible with interoperable systems is crucial for efficient continuity of care, ensuring that patients’ treatments are consistent and accurately documented across all stages of their healthcare journey.
In the intensive care unit, there are dozens of mission-critical medical devices and multiple hospital systems generating and utilizing patient data. Serving as the central connecting element, the clinical information system must be able to receive data from all the systems and devices as well as feed data to the relevant systems, automatically and seamlessly.
High interoperability between the clinical information system and the existing critical care infrastructure can mean the difference between timely, effective interventions and delays or errors that could result in grave outcomes. It also significantly reduces double-documentation, saving time and frustration for clinicians by minimizing the need for them to enter the same clinical information in multiple systems.

Benefits of an automated integrated system in critical care
The need for interoperable systems becomes evident when you consider some of the common scenarios around intake of new patients directly into the ICU and in transition of care situations within the hospital.
Improving medication lists in the ICU
Patients often arrive in the ICU from different wards or from home with a pre-existing list of medications. Often, the ICU clinicians must re-enter this medication data into the ICU’s system or manually compare the information between different systems. In addition to being time-consuming, this kind of double-documentation is also prone to errors, especially in high-pressure situations or during night shifts.
When the ICU clinical information system is integrated with other healthcare systems, medication lists can be automatically communicated across care settings and platforms, ensuring that clinicians have accurate and up-to-date data. This can avoid delays in medication care when patients transition to and from ICU and reduces the likelihood of errors. Interoperability between systems also facilitates quicker adaption of treatment plans based on up-to-date medication information, which is crucial for critical care efficacy.
Streamlining allergy documentation
Allergy documentation is another common issue, with patients’ allergies needing to be documented across multiple systems. When a patient is transferred to a new department, staff often need to ask again about allergies, even if this information was already provided in another part of the hospital.
These kinds of redundancies not only waste time but they also increase the risk of missing crucial information, particularly if the patient is unconscious or their family is unavailable to confirm details – as commonly occurs when patients are admitted to the ICU.
With interoperable systems, the medication list and allergy information can be automatically populated in the clinical information system, ensuring accuracy and saving valuable time for healthcare providers.
Why healthcare interoperability is so challenging
Every modern hospital, including its various clinical departments, functions as a complex ecosystem of numerous systems and devices from different suppliers. This complexity is especially pronounced in the critical care department, which often utilizes the most advanced, best-of-breed systems for monitoring, diagnostics, and therapeutics. The abundance of diverse technologies poses significant challenges for achieving seamless interoperability across the continuum of care.
A major hurdle in achieving interoperability is the existence of multiple standards for transmission of data between different devices and systems. While some standards, such as the HL7® FHIR® (Fast Healthcare Interoperability Resources), are widely accepted globally, some manufacturers of medical devices and systems develop their own proprietary standards. This fragmentation makes it difficult to ensure that systems from different vendors can communicate effectively.
In the field of clinical information management, some systems that are more closed are presented as comprehensive solutions designed from the outset for use throughout the hospital. While these systems may perform many functions adequately, they tend to fall short in handling the more complex, specialized tasks prevalent in critical care environments. In contrast, ICU-specialized systems are designed to excel in meeting the high-stakes, data-intensive demands of critical care. As part of that, the interoperability of the system is paramount.
Building continuum of care through seamless interoperability
Healthcare interoperability is a cornerstone of continuum of care. Integration of hospital systems and medical devices with the clinical information system ensures that clinicians have the comprehensive patient data they need throughout the patient journey, empowering them to make the best-possible clinical decisions for patient safety and optimized outcomes. This seamless connectivity is especially critical in fast-paced environments like critical care, where technology for nurses can further enhance access to real-time data and improve care.
Seamless interoperability is vital for managing transition of care, especially for patients moving between settings and when managing chronic conditions. It ensures that comprehensive patient information follows each patient, supporting treatment continuity and safety across diverse healthcare environments. This not only facilitates coordinated care plans but also enhances collaborative decision-making among healthcare professionals, crucial for effective case management.
How iMDsoft supports the continuum of care, with MetaVision
MetaVision stands out as a critical care-focused clinical information system designed from the ground up for interoperability. Because MetaVision’s interoperability capabilities are a cornerstone of its design, it excels in supporting the continuum of care across various departments and even different hospitals within the same network. With MetaVision, a single patient record can be shared throughout an institution, ensuring clinicians have access to comprehensive patient data from previous and current admissions, as well as planned future care.
Interoperability in MetaVision goes right down to its system architecture, which is designed to enable seamless, secure communication across the range of hospital systems. The system fully supports smooth data exchange, utilizing standards like HL7® FHIR®, HL7 Messaging, HL7 Clinical Document Architecture (CDA) and ASTM. It offers an extensive set of FHIR interfaces, including FHIR Observations, FHIR MedicationDispense, FHIR MedicationRequest, FHIR Patient, and more.
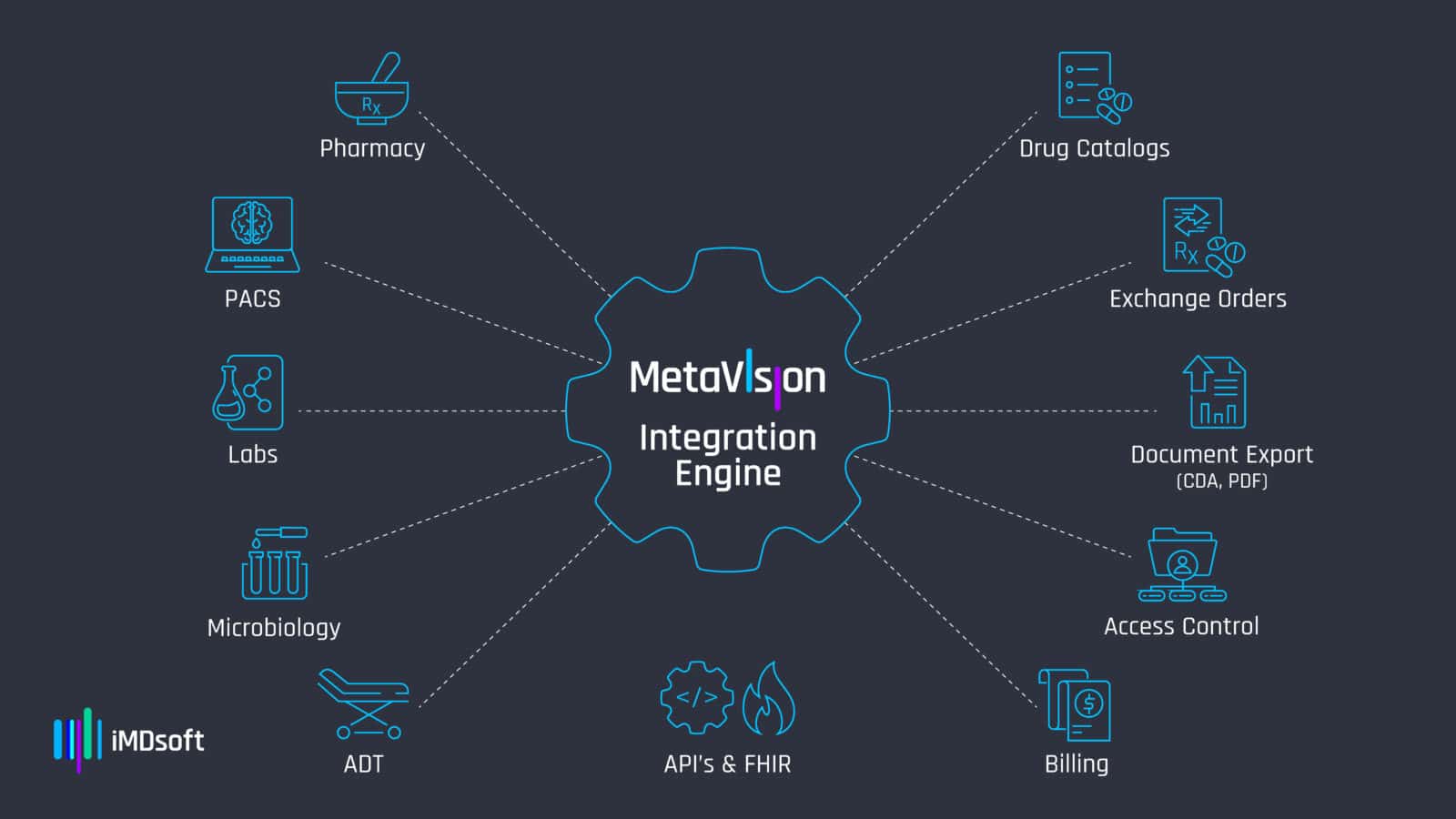
The extensive interoperability provided by MetaVision enables clinicians to efficiently access complete, up-to-date patient information through a single interface, supporting properly informed decision making. Along with that, it significantly reduces the burden of double-documentation, allowing for efficient, accurate, and comprehensive patient care.
Key takeaways
- The goal of interoperability is to provide timely and seamless portability of information, so that clinicians have the right information at the right time to make the best possible decisions for patient care.
- Interoperability between hospital systems and devices is vital for providing high-quality critical care, and the clinical information system provides the essential linchpin. A highly interoperable clinical information system can drive numerous benefits.
- High interoperability between the clinical information system and the existing critical care infrastructure can improve quality of care and patient outcomes.
- Seamless data integration ensures clinicians have immediate access to comprehensive, up-to-date patient information, facilitating improved decision-making, supporting continuum of care and helping improve patient safety.
- Interoperable systems save time by minimizing redundant tasks and manual entry of data.
- Closed systems tend to fall short in handling the more complex, specialized tasks prevalent in critical care environments.
FAQs
-
What is interoperability in healthcare?
Interoperability in healthcare refers to the ability of different information systems, devices, and applications to access, exchange, and integrate data, allowing clinicians to have the right information at the right time for optimal patient care.
-
Why is interoperability crucial in the ICU?
In the ICU, interoperability is vital because it enables the seamless exchange of data between various critical medical devices and systems, reducing errors and ensuring timely and effective patient interventions.
-
What challenges exist in achieving interoperability?
Major challenges include the use of multiple standards for data transmission, proprietary systems from different vendors, and the complexity of integrating diverse technologies within a hospital's ecosystem.
-
How does MetaVision support interoperability?
MetaVision is designed for high interoperability, supporting seamless and secure data exchange across various hospital systems using standards like HL7® FHIR® and HL7 Messaging, ensuring comprehensive and up-to-date patient information is accessible to clinicians.





 Back to lobby
Back to lobby